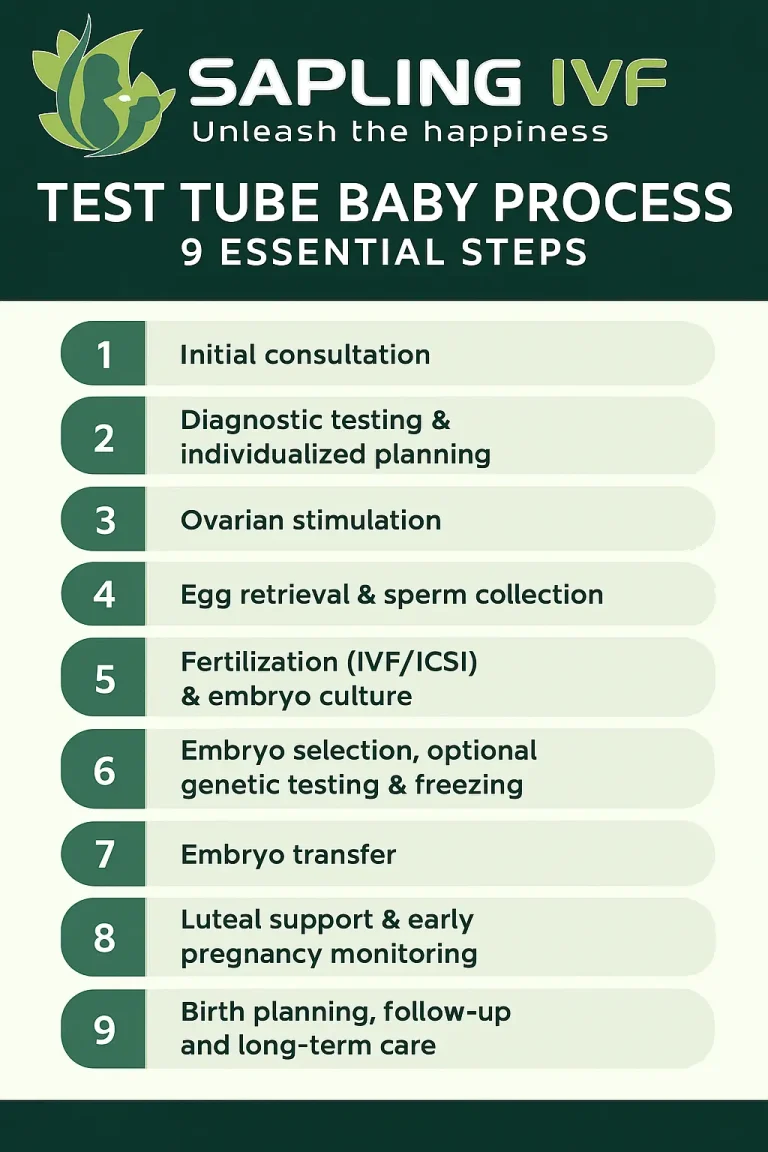
Quick overview — Test Tube Baby Process
First, the test tube baby process begins with assessment and planning.
Second, diagnostic testing informs personalized stimulation.
Third, eggs are retrieved and fertilized (IVF/ICSI) and embryos are grown.
Fourth, the best embryo is transferred and luteal support follows.
Finally, pregnancy testing, follow-up, and birth planning complete the pathway.
Introduction: What is the Test Tube Baby Process?
The test tube baby process (commonly known as in-vitro fertilization or IVF) is a medically assisted pathway that helps people conceive when natural conception is challenging. Because this is a life-changing medical decision, we explain each step clearly and compassionately. Moreover, this guide is written to support you with evidence-based facts, practical expectations, and real next steps.
Why the Test Tube Baby Process matters?
Firstly, the test tube baby process gives many individuals and couples a reliable option to build families when other methods have not succeeded. Secondly, because infertility affects physical and emotional health, this pathway often integrates medical, psychological, and reproductive expertise. In addition, modern techniques such as ICSI and embryo culture have improved outcomes. Consequently, people worldwide consider IVF when they want an effective, supported route to pregnancy.
Who can consider the Test Tube Baby Process?
People with tubal blockage or severe endometriosis.
Couples with unexplained infertility after standard investigations.
Individuals with male-factor infertility (for example, low sperm count), where ICSI is often used.
Same-sex couples and single parents seeking assisted reproduction.
Therefore, eligibility depends on individual health, age, and diagnostic results. For detailed clinical evaluation and to choose the right specialist, please see our guidance on choosing an IVF specialist — for example our article about choosing the right IVF specialist in Gurgaon provides practical tips and is worth reading for anyone selecting a team.
Test Tube Baby Process — 9 essential steps (step-by-step)
Below is the stepwise 9-step test tube baby process, explained in patient-friendly language. Each step shows what happens, why it matters, and what you can expect.
Step 1: Initial Consultation
First, you meet your fertility specialist for a comprehensive history and physical exam. Next, baseline tests are ordered, including hormone profiles and ultrasound. Because personalized planning matters, the doctor uses this information to design the stimulation protocol and timeline.
Step 2: Diagnostic Testing & Individualized Planning
Then, both partners typically complete diagnostic tests. For example, women may have AMH, FSH, and a pelvic scan, while men have semen analysis. Moreover, genetic screening may be discussed if indicated. As a result, the team finalizes the medication plan and expected monitoring schedule.
Step 3: Ovarian Stimulation
First, medications stimulate multiple follicle growth so that several eggs can be retrieved. Then, you attend frequent monitoring visits (blood tests and ultrasounds) to track follicle size. Because timing is crucial, your clinic will advise when to trigger final maturation before retrieval.
Step 4: Egg Retrieval & Sperm Collection
Next, eggs are retrieved in a short, image-guided procedure under sedation. Meanwhile, sperm is collected on the same day or sourced from a partner/donor as planned. After retrieval, eggs are immediately handed to the embryology team for insemination or ICSI.
Step 5: Fertilization (IVF/ICSI) & Embryo Culture
Then, eggs are fertilized either by traditional IVF or by ICSI (intracytoplasmic sperm injection) if male-factor issues exist. After fertilization, embryos are cultured in the lab and monitored for quality. Importantly, embryology labs grade embryos to guide selection for transfer.
Step 6: Embryo Selection, Optional Genetic Testing & Freezing
After embryos develop, embryologists select the highest-quality embryo(s). Moreover, if indicated, preimplantation genetic testing (PGT) can be performed to screen for specific chromosomal issues. As a result, clinicians may recommend fresh transfer or freeze embryos for a later frozen embryo transfer (FET).
Step 7: Embryo Transfer
Then, a selected embryo is transferred into the uterus via a simple, guided procedure. Because transfer technique and uterine preparation affect outcomes, clinics optimize lining thickness and hormonal support beforehand. After the transfer, you rest briefly and then resume gentle daily activities as advised.
Step 8: Luteal Support & Early Pregnancy Monitoring
Following transfer, hormonal support (often progesterone) helps maintain the uterine lining. Next, a blood pregnancy test is usually done about 10–14 days post-transfer. If positive, early ultrasounds track pregnancy progression. Meanwhile, your team provides clear plans for follow-up and prenatal care.
Step 9: Birth Planning, Follow-up and Long-Term Care
Finally, after a confirmed pregnancy, routine obstetric care continues with additional support from reproductive specialists if needed. In addition, frozen embryos remain an option for future family expansion, and counselling supports emotional and physical wellbeing throughout.
What to expect with outcomes & safety
Firstly, success rates vary by age, diagnosis, and clinic expertise. Secondly, advances have improved live birth rates, but no treatment guarantees success. Therefore, talk openly with your team about realistic expectations and possible next steps after a failed cycle. Moreover, safety is high when procedures are performed by accredited teams in modern labs.
Practical Checklist
Book a detailed consultation and bring previous test results.
Start lifestyle optimization (balanced diet, smoke-free, controlled weight).
Prepare questions for your clinician about medications, timelines, risks, and costs.
Discuss emotional support and counselling options.
Because preparation improves experience, use this checklist to arrive informed and ready.
Choosing Your Clinic & Expert Team
First, prioritize clinics with accredited embryology labs and experienced specialists. Second, consider aftercare, counselling, and transparent pricing. For more on selecting the right specialist, read our practical guide on choosing an IVF specialist in Gurgaon which explains how to evaluate credentials and patient experience.
In addition, you can learn about the specific protocols we offer by visiting our IVF services page to explore detailed IVF treatments and protocols available at our centre.
Conclusion & Next Steps
In summary, the test tube baby process is a structured, evidence-based route to parenthood that involves nine clear steps from assessment to birth planning. Therefore, if you are considering IVF, the best next step is a specialist consultation to personalize care.
Book a consultation at Sapling IVF Centre in Delhi and Gurgaon to discuss your test tube baby process plan and timelines; our team will guide you through each step with clinical expertise and compassionate support.
FAQs: Test Tube Baby Process
The test tube baby process usually takes 4–6 weeks per cycle, beginning with consultation and ovarian stimulation, followed by egg retrieval, embryo transfer, and a pregnancy test. Timelines may vary depending on individual health and whether fresh or frozen embryos are used.
Success rates for the test tube baby process depend on age, fertility diagnosis, and clinic expertise. On average, women under 35 may have a 40–50% live birth rate per cycle, while older age groups may have lower rates. Discussing personalized expectations with your fertility doctor is crucial.
Most parts of the test tube baby process are not painful. Ovarian stimulation may cause mild bloating, while egg retrieval is performed under sedation to avoid discomfort. Embryo transfer feels similar to a routine gynecological procedure. Any side effects are usually mild and short-term.
The test tube baby process is generally safe, but some women may experience temporary bloating, mood changes, or mild cramping. Rare risks include ovarian hyperstimulation syndrome (OHSS) or multiple pregnancies. Choosing an experienced clinic reduces these risks significantly.
The cost of the test tube baby process in India typically ranges from ₹1.5 lakh to ₹2.5 lakh per cycle, depending on the clinic, medications, and whether advanced techniques like ICSI or genetic testing are used. Many clinics offer payment plans to make treatment accessible.

